Imagine strolling through life with a blind spot so sneaky it could hide from a magician. Loss of peripheral vision might sound like a minor inconvenience, but it can turn everyday activities into a game of dodgeball. What’s lurking in those shadowy corners? The neurological culprits behind this condition can be as diverse as they are surprising.
From pesky migraines to more serious conditions like glaucoma, understanding the neurological causes of peripheral vision loss is crucial. It’s not just about seeing the whole picture; it’s about staying safe and aware in a world full of unexpected surprises. Buckle up as we dive into the brain’s mysterious workings and uncover what might be dimming your view.
Table of Contents
ToggleOverview of Peripheral Vision
Peripheral vision refers to the ability to see objects outside of one’s direct line of sight. This vision uses the retina’s peripheral regions, where rod cells dominate, aiding in detecting motion and light. Often, these regions detect shapes and movements, providing crucial situational awareness.
In everyday life, individuals rely on peripheral vision to navigate environments and avoid obstacles. For instance, while driving, peripheral vision helps identify vehicles and pedestrians outside the central focus. The brain processes this visual information to create a comprehensive picture of one’s surroundings.
Various neurological factors contribute to peripheral vision loss. Conditions such as glaucoma can damage the optic nerve, leading to reduced field of view. Additionally, strokes or brain injuries can impede the areas responsible for processing peripheral vision in the visual cortex.
Beyond medical conditions, migraines can affect peripheral vision temporarily. This phenomenon, known as a visual aura, may present as flickering lights or blind spots. These episodes often resolve but can create confusion in daily activities.
Understanding these causes can significantly impact one’s awareness and safety. Recognizing the symptoms early allows for timely assessments and interventions. Individuals experiencing peripheral vision changes should seek professional evaluations to determine underlying neurological issues. Through awareness and understanding, they can better manage their condition and enhance their quality of life.
Neurological Anatomy Involved
Neurological anatomy plays a vital role in understanding peripheral vision loss. Several key areas within the visual pathway contribute significantly to this condition.
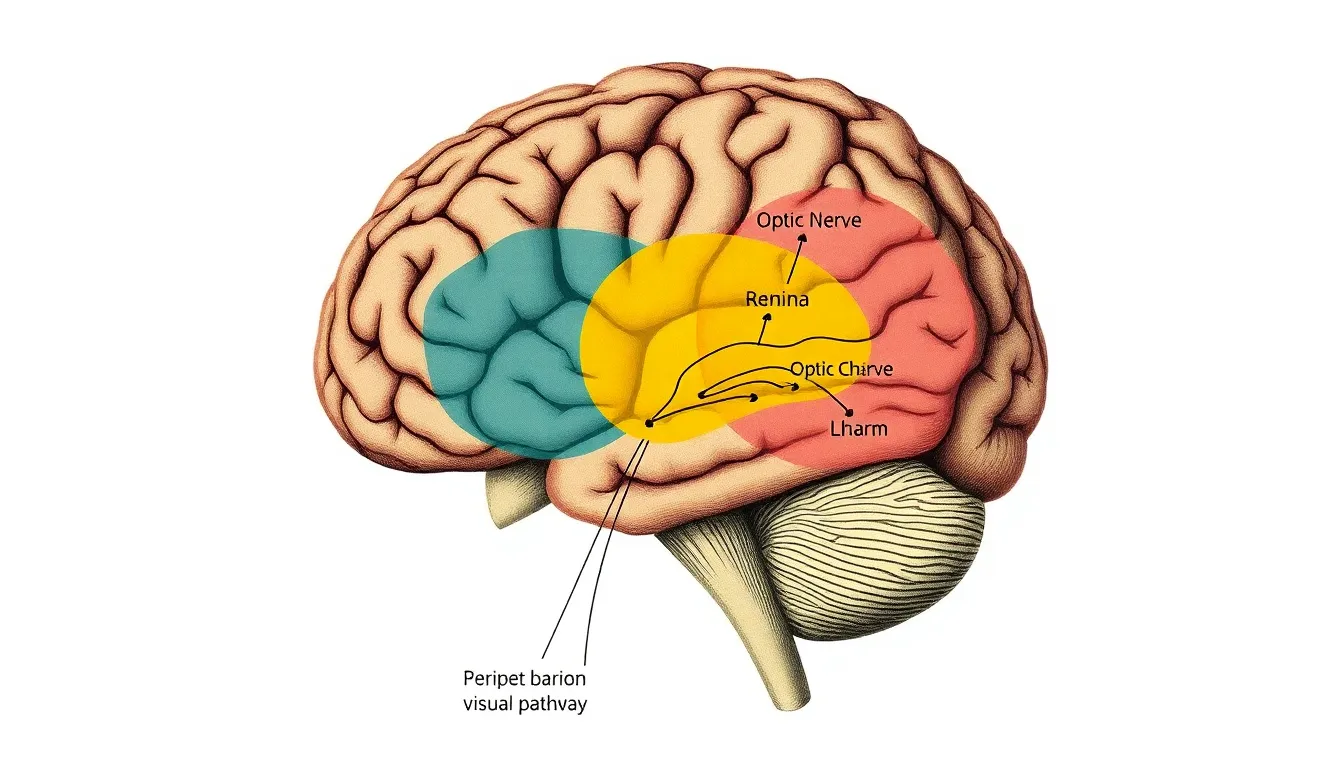
Structure of the Visual Pathway
The visual pathway begins with the retina, where light signals initially convert into neural impulses. These impulses travel through the optic nerve, which connects each eye to the brain. From the optic nerve, fibers cross at the optic chiasm, allowing visual information from both eyes to merge. After the chiasm, the optic tracts extend to the lateral geniculate nucleus (LGN) of the thalamus. Relay neurons then transmit signals from the LGN to the primary visual cortex in the occipital lobe, making this entire pathway essential for peripheral vision. Damage at any point along this route can lead to significant vision loss.
Role of the Brain in Vision
The brain processes visual information through complex interactions within multiple regions. The occipital lobe serves as the primary processing center, interpreting signals received from the LGN. In addition to the occipital lobe, the parietal lobe engages in spatial awareness, while the temporal lobe integrates visual data with other sensory inputs. These areas work collaboratively to construct a cohesive visual experience. Disruptions in these regions may result in difficulty detecting objects along the periphery, underscoring the importance of the brain’s involvement in maintaining comprehensive vision. Understanding these anatomical functions enhances the approach to diagnosing and addressing peripheral vision loss.
Common Neurological Conditions
Various neurological conditions can lead to peripheral vision loss. Understanding these conditions helps in recognizing symptoms early.
Glaucoma and Its Connection
Glaucoma significantly affects peripheral vision through increased intraocular pressure. This pressure damages the optic nerve, leading to gradual vision loss. Early stages of glaucoma may not present symptoms, making routine eye exams essential for detection. With proper management, individuals can slow the progression of this disease and preserve their vision.
Multiple Sclerosis
Multiple sclerosis (MS) explores the central nervous system, causing damage to the optic nerves. This demyelination often results in visual symptoms, including peripheral vision loss. Individuals with MS may experience blurred or double vision, emphasizing the need for early intervention. Treatments like corticosteroids and disease-modifying therapies are available to manage symptoms and improve quality of life.
Stroke and Vision Loss
Stroke represents a significant cause of vision impairment, particularly in peripheral fields. When a stroke occurs, it can affect the brain areas responsible for visual processing. Individuals may experience homonymous hemianopia, where vision loss occurs in the same field of both eyes. Timely rehabilitation can assist in adapting to changes and improving functional vision after a stroke.
Diagnostic Approaches
Diagnostic approaches for peripheral vision loss leverage clinical assessments and imaging techniques to uncover underlying neurological causes. Recognizing specific symptoms helps guide these evaluations, ensuring accurate diagnoses and effective management.
Clinical Assessments
Ophthalmologists and neurologists conduct various clinical assessments to evaluate peripheral vision. Visual field tests determine the extent of vision loss, identifying blind spots or areas of diminished sensitivity. Additionally, a comprehensive eye exam assesses the health of the retina and optic nerve, revealing potential damage. Neurological exams test reflexes, coordination, and overall visual processing capabilities. Gathering patient history, including any recent neurological events, informs the diagnostic process.
Imaging Techniques
Imaging techniques play a crucial role in diagnosing causes of peripheral vision loss. MRI scans offer detailed views of the brain’s structures, highlighting abnormalities affecting visual processing. CT scans serve as an alternative, providing insight into structural damage or bleeding. Furthermore, optical coherence tomography evaluates the retina’s layers, detecting issues related to glaucoma or macular degeneration. These imaging methods, combined with clinical assessments, create a comprehensive understanding of the patient’s condition, facilitating targeted treatments.
Treatment Options
Several treatment options exist for addressing peripheral vision loss caused by neurological issues. Medical interventions and rehabilitation strategies play critical roles in managing this condition.
Medical Interventions
Medications may help treat underlying causes, such as glaucoma, where eye drops lower intraocular pressure and prevent further vision loss. Corticosteroids can reduce inflammation in conditions like multiple sclerosis. Surgical procedures, including laser therapy, may also eliminate obstructions and improve peripheral vision. In some cases, addressing the root cause, like stabilizing blood sugar in diabetes, can prevent additional vision impairment and enhance overall sight. Regular follow-ups with healthcare professionals allow for monitoring progression and adjusting treatment plans accordingly.
Rehabilitation Strategies
Rehabilitation focuses on maximizing the remaining vision and improving quality of life. Orientation and mobility training equip individuals with skills to navigate their environment confidently. Vision therapy exercises enhance visual processing and tracking skills, aiding in situational awareness. Specialized glasses or visual aids help individuals make the best use of their existing vision. Support groups provide a platform for sharing experiences and coping strategies. Creating a plan tailored to one’s unique needs enhances daily functioning and promotes adaptability.










